End of life is a heart-breaking and difficult time for all those who experience it. Families, friends and I’m sure also medical teams who may be involved. What sad news it was to read of a friend who had lost both his parents just eight days apart during March. One can’t fail to not just sense the feeling of loss that this friend must be feeling but also to sense that familiar sorrow you feel for your missing loved ones. For me it’s that huge void left from my mother departing over 3 years ago. Of course everyone in the family was effected but one was impacted in such a way that it took her on an amazing journey that transformed her life.
One thing I learnt from my mum was that we all have within us a purpose for our life. That when we depart we would have wanted to make our mark and leave a legacy.
Well my youngest daughter is one of my mum’s greatest legacies. She is now in her last year of her nursing degree. She chose this career as a culmination of my mums passing and the events that led up to this.
In a way it led her, my daughter, to finding her life’s purpose. Something that has become her calling. In fact right now I imagine her beavering away in the library at the University she’s attending writing up her dissertation.
Her topic is end of life care – specifically communication with relatives in end of life care.
End of life care is an important part of palliative care for people who are nearing the end of life. To help people live as well as possible and to die with dignity. It also refers to supporting the families through this difficult period.
Behind this lies a story. And a decision that my daughter made that would not only change her life but will I have no doubts change the lives of others in the future. Let me explain and further support what it is she’s driven by.
You see, when my mother was ill in hospital, the doctors and nurses although many did show good care to my mother, their communication was lacking, to say the least.
We were often completely in the dark.
Worse at other times we were confused and puzzled by what we were told.
For a month no one would give us a diagnosis, tell us what was wrong with her, in fact they all seemed to avoid the subject. We were by her side nearly every day. She was in a deep sleep. Not a coma, not unconscious, simply sleeping. She didn’t wake up. She was breathing normally. Snoring as well. Maybe for 5 minutes every couple of days she say a word or two, then back to sleep.
We didn’t know what was wrong, why she was in this state, or even if there was the possibility of her waking up, which just gave us additional unnecessary stress.
We weren’t even informed if they were able to do anything to wake her up. All we could ascertain was they were constantly doing checks on her.
Communication was sketchy. Medical updates non-existent. We would be asked to leave on doctors rounds, but rarely after our return would we be told anything. Every day we seemed to have to find a nurse and ask her if the doctor had found anything. There was no body seemingly willing to take the responsibility to provide us with daily information nor provide us the opportunity to clarify anything.
Of course it has to be the medical team’s number one priority to look after a person fighting against serious illness or even imminent death, to provide them with excellent end of life care; but you would hope they would provide good, clear and straightforward information to their families in regard to their end of life care.
It is understandable if there is discomfort in having difficult conversations with the families particularly when things are looking bleak, and end of life is expected. They fear upsetting the family members and may be reluctant to initiate such a discussion. They realise the likelihood that family members will be stressed and confused by their situation and on edge with their emotional burdens. But they need to realise this stress is heightened by a lack of knowledge. It drove us crazy.
Good communication would surely make the whole process better, giving everyone an understanding to what’s happening. There can be nothing worse than receiving little updates, with the confusion and uncertainty this brings. In my mind, having gone through what we did, it would have been far better being fully informed about everything and not left to guess as events unfolded.
Talking of confusion. One of the many visits to the hospital – a doctor who we had never seen before asked me and my youngest daughter to go into a little room in the corner of the ward to speak to us. I will never forget this conversation. She informed us that she had put my mother on a DNR and had started her on the Liverpool care pathway to make her comfortable. We were in shock, particularly my 15 year old daughter. No one has told us to prepare for this. And no one even explained to us what this pathway was or what this meant? I had to google it afterwards on my phone. This is a delicate situation handled badly that could have resulted in long-term psychological consequences which fortunately in our case didn’t but I’m sure others haven’t been as fortunate.
It was obvious how breaking bad news, particularly discussing prognosis, requires excellent communication skills which wasn’t something this doctor had been trained to do well enough.
It didn’t end there though. I had similar conversations over the next 6 weeks or so with various doctors who kept taking her off the pathway and putting her back on. Not one of them had an open and honest conversation with us, no one said the words ‘your mother is dying’. Nor did they ever tell us what had actually happened, or what was happening to keep her in an almost permanent sleep.
Then out of the blue she was allowed to be bought home. After nearly three months in hospital and being on and off the pathway she was highly malnourished and had lost a lot of weight. I did my research on this pathway and normally if people are on it it’s because they’re meant to not last no more than a few days. We thought she came home as she was getting better. No one told us she came home to die. So when she did within a week of being back, you could say although a slight relief as now she was not suffering, it made our grieving process worse and as a family we hadn’t been prepared for my mum’s death.
Afterwards nobody ever explained what happened or answered any questions. We really never did gain closure about anything that we all went through for those 3 months.
Like I said the care she received was good the majority of the time but the communication was seriously lacking.
We were never provided regular opportunities for communication or be put in a situation where we understood or were updated about her condition, treatment and or care given to our mum.
Since those days, nearly three years ago, my daughter has informed me that the Liverpool care pathway has now been removed as ‘it was being misused’. I really hope that no one would have to go through this. I know that because my daughter did, it was the motivation behind her deciding to become a nurse and this experience I have no doubts will endure nobody under her care will ever be treated this way.
It is my conclusion that end of life care is not something that doctors or nurses are taught about well based on my own personal experiences and is something that appropriate training needs to be given. Constant, concise, sensitive and effective communication is vital to ensure everyone understands what is happening and why decisions have been made. Well trained and professionally competent medical teams providing high standards of communication to patients and their families at the end of life care will make a huge difference as will providing support, comfort and understanding at such a challenging time.
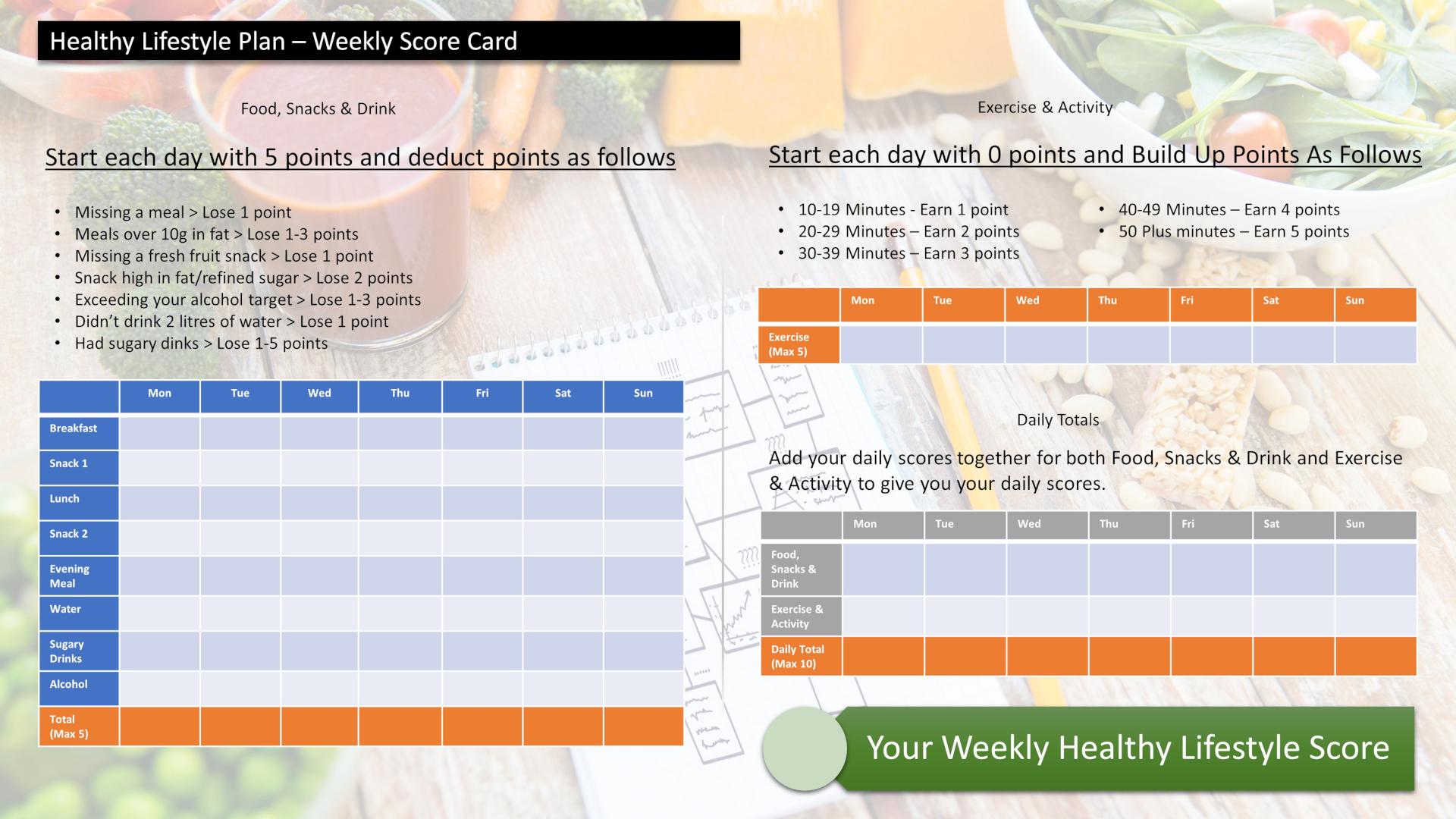
Score Your Way To Good Health - With Our Healthy Lifestyle Plan
Score your way to good health with our healthy lifestyle plan and it's unique 70 point weekly scorecard!